- The Arrow
- Posts
- The Arrow #267 Rosy Cancer Stats, US Life Expectancy
The Arrow #267 Rosy Cancer Stats, US Life Expectancy
Hello everyone and greetings from sunny SoCal. It’s a beautiful day in the neighborhood. There was nothing much in the emails or comments I need to address this week, so let’s move right on.
Rosy Cancer Stats
Did you see the news a couple of weeks ago about the American Cancer Society’s release of its annual report on cancer facts and trends? The new report shows that the US five-year relative survival rate for all cancers combined reached 70% for people diagnosed in the half decade between 2015 and 2021. Especially noted were what were viewed as strong gains against cancers with some of the worst prognoses, such as myeloma, liver cancer, and lung cancer. Great news, right? Or is it?
Rebecca Siegel, senior scientific director of surveillance research for the ACS and lead author of the report said in commentary:
“Seven in 10 people now survive their cancer five years or more, up from only half in the mid-70s…This stunning victory is largely the result of decades of cancer research that provided clinicians with the tools to treat the disease more effectively, turning many cancers from a death sentence into a chronic disease.”
While there have been undeniable gains for better survival of some cancers, they’re mainly the slow-growing, indolent ones, or the easily diagnosed and accessible ones (thyroid, prostate, testicular, and melanoma), and great gains have been made in surviving blood cancers, but how much of the ‘stunning victory’ is actually the result of what Rebecca Siegel said — providing clinicians with tools to treat effectively? And how much to simply finding cancers in earlier and earlier stages? And to combining the statistics of very survivable/curable cancers, such as those mentioned above, with the much poorer response of the more lethal ones. The treatable ones have 95% and 98% 5-year survivals and the more lethal ones still down in the 20% to 25% range.
The cases of my lovely Bride’s family are illustrative of what I’m talking about.
Finding Cancer
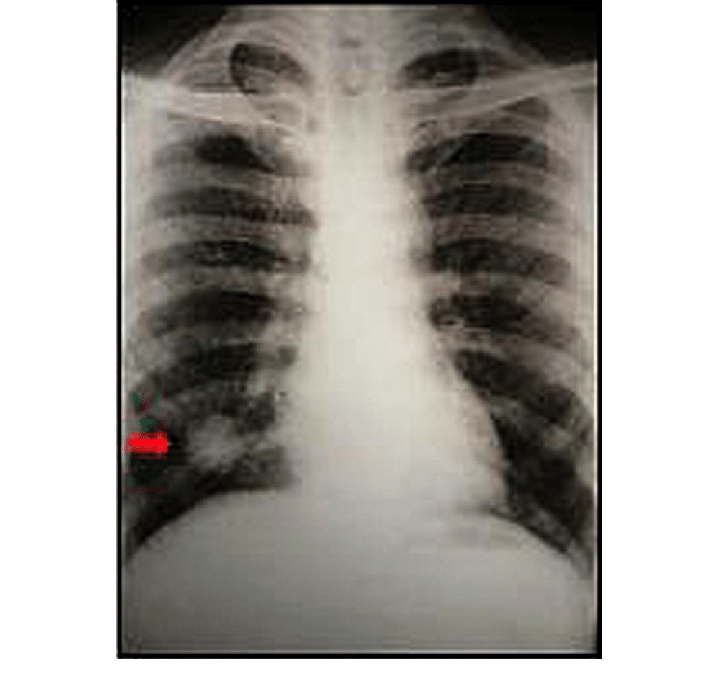
Back in the late 1970s, MD’s mother was diagnosed at age 50 or 51 with a highly undifferentiated adenocarcinoma of the lung. She had no symptoms, and the cancer was diagnosed incidentally on a routine chest x-ray she took annually to prove she didn’t have tuberculosis; she was a teacher and as a person who did not react to the TB skin test, an annual chest x-ray was required.
One year the x-ray turned up what’s known as a ‘coin lesion’ in the upper lobe of her right lung. The name says it all – it’s a bright white perfectly round spot on the lung. The doctors at first assumed it was a metastasis from an adenocarcinoma elsewhere (Breast? Colon? Where?) but further evaluation didn’t turn up anything anywhere else. It was so highly undifferentiated that they couldn’t even identify the cell type (lung, breast, colon, whatever) and this was in the days before they could tissue type from the various antigenic markers that allow them to make such identifications now.
She underwent thoracotomy with removal of the upper and middle lobes of her right lung, leaving only the lower lobe on that side along with the misery of recovering from open chest surgery. And they followed up with radiation treatments locally and to her head prophylactically even though nothing suspicious had yet shown up. (This was in the days before PET scanning could pinpoint a cancer’s locations through discovering its metabolic activity thanks to its pronounced love of glucose, in this case of taking up radioactively-labeled glucose.)
Over the next year, she underwent repeated tests (mammograms, colonoscopies, barium enemas, pelvic/pap tests, etc.) in search of that suspected primary tumor, all without success. And then she developed a bad headache that she thought was a sinus infection, but that turned out to be a large brain metastasis of her lung tumor. She underwent brain surgery to remove the tumor, followed by more head radiation.
And then in about a year, she developed headaches again and testing showed it was new brain metastases. She underwent another operation to remove them (around Thanksgiving that year) that happened to coincide with my stint as a surgery resident on an anesthesia rotation. I was actually in the OR during the case, when the head of neurosurgery and another staff neurosurgeon, who was a friend of mine and MD’s, declared they’d gotten the last visible bit of tumor. All the mets were gone on scans.
In a couple of months, the mets were back with a vengeance, the scans showing 4 or 5 of them scattered throughout her brain. Despite a couple of cycles of chemo, which they had to stop because her blood counts plummeted dangerously low, she died of her disease in April at age 55.
So technically, she had survived 5 years from the time of her first diagnosis, at a time when the 5-year survival of lung cancer hovered between 12 and 15%. (Now it’s said to be about 25% or so.) But what if she hadn’t been diagnosed early? What if she hadn’t been diagnosed until she developed the headaches? The two years between her original incidental diagnosis and her headaches that showed a brain met were filled with painful procedures and little joy.
Now, contrast that case with a much more recent one – MD’s sister. We had gone to visit her after Christmas in 2011 and stayed through until January 2, 2012. She had seemed her usual self, but as we were leaving to drive back to Dallas, she told MD she had a bit of a sore throat and cough and thought she was coming down with something and could she call in a prescription for an antibiotic to knock it out? MD did that. It didn’t knock it out, and a couple of weeks later her sister asked for a refill. MD did that, but told her sister that if this round didn’t put her right, she needed to be seen by someone who could listen to her chest and look in her throat and maybe get a chest x-ray.
She promised she would make an appointment, but in the interim, a doctor associate of hers on the Arkansas State Medical Board (she was a community representative on the board) mentioned that there was some respiratory thing going around, and that nothing but Levaquin would knock it out. So she called MD and asked for a prescription for that antibiotic. Which she gave her, but again with the admonition that she needed someone there to look and listen.
And then a week or two later her sister was on the phone speaking to a retired anesthesiologist friend, when she fainted, fell, and dropped the phone. He lived nearby and rushed to her house. By the time he got there she was ‘back’ and still weak, but able to let him in. He took her to the ER where they did a chest x-ray that was read as unremarkable other than her mediastinum (the space sort of between the lungs) seemed a bit wider than normal. So they arranged a chest CT for a week or so later.
She finally made a doctor’s appointment but when the day came, she felt bad enough that she called her nephew to drive her. When they got to the office to check in she couldn’t sign her name, couldn’t remember how to do it. She was to see the doc’s PA, but her nephew insisted that this was something much bigger than a chest cold and sore throat and they saw the doctor instead, who admitted her to the hospital for testing.
So we are into early March now, and in about two months she’s moved from feeling like herself to can’t write her name. And the body scans done in the hospital showed she had widely metastatic cancer, in her mediastinum, in her hilum, in her adrenal glands, and in her brain, which were causing her sudden symptoms. Skinny needle biopsy of one of the mets identified the cell type as highly undifferentiated adenocarcinoma of the lung, the exact same cell type as her mother’s likely was. Though no lung lesions were ever seen.
Her sister wanted to ‘pull out the stops’ as she told her oncologist, and in the next months she underwent a course of many packets of radiation to her head and then to her chest, and once that was finished she began a course of weekly cisplatin chemotherapy. She managed about 5 doses of that before developing toxicity that required stopping the therapy. Along the way, she developed a bleeding gastric ulcer (from surreptitiously taking a lot of ibuprofen for pain) that necessitated another hospital stay and then a deep vein thrombus that required placement of an inferior vena cava filter and yet another hospital stay.
Scans done on May 15th showed regression of the hilar and mediastinal nodes by about half and that the brain mets had shrunk significantly. On June 2nd MD spoke to her sister’s oncologist (MD had come back to California for a week after being there with her sister for the last month or so) about discharging her to a rehab facility (which he recommended) versus sending her home with visiting nurses (which is what she wanted). MD had heard from her nephew how weak her sister still was, and so she asked the doc to please while he was in the room with her have her get herself out of the bed unaided and get to the bathroom (steps away). She couldn’t do that yet. So he told her his rule was that to go home, she needed to be able to get herself out of the house on her own if it were to catch fire. And right now she couldn’t do that. So he made arrangements to transfer her to a rehab hospital for a few weeks of PT and strengthening.
And the very next morning, he called MD and told her to come immediately. That he was on the way to the hospital and things looked grim – he called it ‘lymphangitic swarm’ of the cancer. He said she wouldn’t last long. She died that evening just before the car arrived in Santa Barbara to take us to the airport to fly back there.
So, in this case, the earliest symptoms began January 2, though those could really have been just a cold. Major symptoms pointing to something big going on and the subsequent diagnosis happened March 5, and she was dead after ‘pulling out all the stops’ on June 3. So three months survival? Maybe five if you take it back to January. And around $400,000 in Medicare billing.
What if her disease had been discovered incidentally (as her mother’s had been) three, four, five years earlier? Would her course have been different? Would it have altered the ultimate trajectory of this cancer? Would she still have died in June of 2012, but now as a 5-year survival success, after multiple surgeries, radiation, chemo, and misery in the intervening time?
And what might she have missed out on?
MD, her sister, my sister, and I had all traveled the summer before to Spain on one of MD’s Choral Society international performance tours and then followed that on our own with a week in Paris. Her sister got to visit Giverny (Monet’s home) which was a bucket list destination for her. We walked all over Spain and Paris, and she was able to do that. Would that have been the case if the years previous had been filled with surgeries, scans, radiation treatments, and chemo?

MD and her sister at an overlook of Toledo, Spain
We don’t know. But it’s worth considering that this rosy new high water mark of a 5-year survival of ‘70% for all cancers combined’ could at least in part be accounted for by finding these lethal cancers earlier and instituting treatment that in the end doesn’t really extend life, but merely extends treatment time. And dollars.
Then one more quick one.
I may have written about this one in times past, but I’ll repeat it. The brother in law of one of our clinic nurses was diagnosed with esophageal cancer back in the mid to late 1980s. His internist, who had to give him the bad news, was a friend of his. A nice guy and an excellent doctor. He told him the situation and said, “John, just go fishing. Go enjoy whatever life you have left.” And that really ticked John off. Instead of going fishing, he went to MD Anderson (the world class cancer institution in Houston, TX) to ‘pull out all the stops’.
He underwent a series of painful surgeries to remove part of and re-attach his esophagus, then radiation, and chemo (as I recall). The side effects from all of it left him miserable, but in a few months they declared him ‘cancer free’. Jubilation! And in another month or so, he was dead of his disease. What if his cancer had been somehow discovered incidentally before he had symptoms? Would it have made any difference to the final course of the disease? I don’t know. Probably not, particularly not in 1980, before the advent of the newer, targeted immunotherapies.
There are some cancers that are more amenable to ‘cure’ or at least long term control if found very early – testicular cancer, colon cancer, cervical cancer, melanomas, thyroid cancer, and some breast cancers come to mind. But a lung, esophageal, pancreatic, or liver cancer by the time it’s big enough to be seen on an x-ray or scan has been around a while and is less likely to be one of those easily treated if caught early ones. There are some long-term survival successes, but nowhere near 70% for these.
The Arrow is a reader-supported publication. If you would like to support my work, please do take out a premium subscription (just $6 per month)—it’s cheaper per month than one Starbucks Vente double pump caramel latte or whatever. And a lot better for you. It will run your IQ up instead of your insulin. And I’ll be very thankful.
US Life Expectancy
And while I’m on the subject of survival, today’s paper brought a headline I thought interesting from the CDC: US Life Expectancy Hits High in 2024.
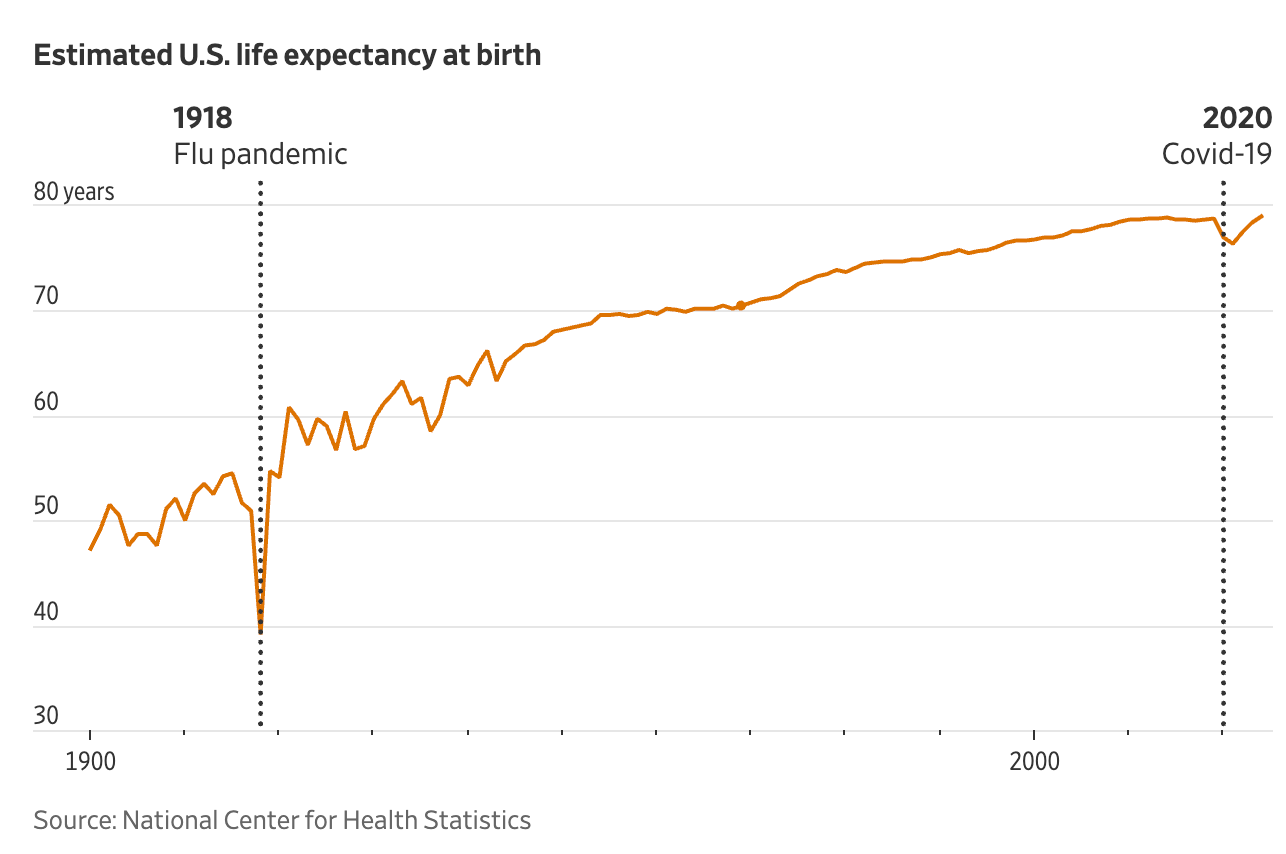
The article goes on to tell us that life expectancy for US citizens in 2024 rose to 79 years, the highest ever in American history. Life expectancy, an estimate of the average number of years a baby born in a given year might expect to live, given death rates at that time, rose slowly and steadily until about 2019, when it topped out near 79 years, but then declined sharply in the wake of Covid-19 deaths, which disproportionately felled the elderly.
So, now it’s rebounded to where it was pre-pandemic, with deaths declining across all racial groups in both genders. Deaths from heart disease (still the nation’s biggest killer) dropped by about 3% which the article attributed to advances in medical treatment and weight management (assuming here they mean Ozempic and Wegovy). (OK maybe, but they could have done the same with a well-formulated, low-carb, ketogenic diet. Just sayin’.)
But the biggest improvement (14%) wasn’t the result of better management and prevention of chronic disease, rather it was from a huge drop in the number of ‘unintentional accidents’ which includes opioid overdoses (Fentanyl, Oxy, and heroin) which disproportionately affect younger people, young men especially. Some of that may be a reflection of less of the stuff coming into the country and the rest from aggressive local programs to make Narcan (naloxone) nasal spray available now without prescription in all 50 states since 2023. That availability allows on scene friends and family to resurrect overdoses before they become fatalities.
Just as the wave of Covid-19 deaths in the elderly dropped the life expectancy in 2021, preventing the deaths of young people from overdose since 2023 will up the life expectancy. Is it a reflection of making the populus healthier? Not really.
So imagine what may happen to the life expectancy number with implementation of the new ‘upside down’ meat-centric food pyramid HHS introduced recently. It will take some time, but that’s a solution to chronic disease prevention that will really make inroads if vigorously adopted. It will be interesting to see what the life expectancy number is in 2030.
Odds and Ends
The oldest, deepest, fullest freshwater lake in the world. Where is it?
Speaking of Siberia, why is snow whitThe Bride and I have noticed this regrettable trend. What's the deal with hotel bathroom doors?
Coolest museum in every state. Have been to a handful of these. Can confirm Crystal Bridges is worth the visit.
Musical mistakes in famous recordings that artists left in the final cut on purpose. I admit I couldn't find the first one no matter how many times I listened. The Bride couldn't either, even with her greater experience of hours of her misspent youth trying to hear the 'Paul is dead' secret lyric by spinning Revolution Number 9 backward on the turntable.
Giant, mysterious spires ruled the Earth long before trees did. What Exactly Are These Odd-Looking Fossils?
The Bride and I had the pleasure of a private tour of the White House back in 1997 with Rex Scouten in the last year of his nearly 50 year tenure as White House Chief Usher and Curator. It was an amazing experience; one we'll never forget. Here's a bit of what we saw.
With ai about to disemploy lots of copywriters and code writers and fast food employees, here are some odd jobs they might look into.
Video of the Week
I stumbled across this terrific video on Twitter a couple of months ago and have been waiting for a good time to put it up. Now is as good a time as any.
My ancestors were Borderers, who came from the area between northern England and southern Scotland. They were an onery bunch, so they ultimately got run out of their homeland and went to Ireland. Then they got booted from there and went back to where they came from. Ultimately, they ended up in the US in Appalachia.
Then in the late 1800s, my specific branch of the family migrated from Tennessee to the Ozark mountains of southern Missouri, where I grew up as a boy.
These kids are still in eastern Tennessee. What I love so much about this video is its authenticity. I’ve seen countless little throw together bands like this back there. I don’t know if these kids are all family, or what, but I could watch this video over and over and over. The dog makes it perfect.
I hope you enjoy it as much as I have.
Time for the poll, so you can grade my performance this week.
How did I do on this week's Arrow? |
That’s about it for now. Keep in good cheer, and I’ll be back soon.
Please help me out by clicking the Like button, assuming, of course, that you like it.
This newsletter is for informational and educational purposes only. It is not, nor is it intended to be, a substitute for professional medical advice, diagnosis, or treatment and should never be relied upon for specific medical advice.
Thanks for reading all the way to the end. Really, thanks. If you got something out of it, please consider becoming a paid subscriber if you aren’t yet. I would really appreciate it.
Finally, don’t forget to take a look at what our kind sponsors have to offer. HLTH Code, Precision Health Reports, and Jaquish Biomedical.
And don’t forget my newest affiliate sponsor Lumen. Highly recommended to determine whether you’re burning fat or burning carbs.

Reply